Continuous Glucose Monitoring (CGM) offers real-time tracking of glucose levels in pets, providing more comprehensive data than Traditional Blood Glucose Monitoring, which relies on periodic, invasive blood samples. Wearable CGM devices enhance pet comfort and enable early detection of glucose fluctuations, improving diabetes management. This technology reduces stress for both pets and owners by minimizing the need for frequent finger pricks and manual data logging.
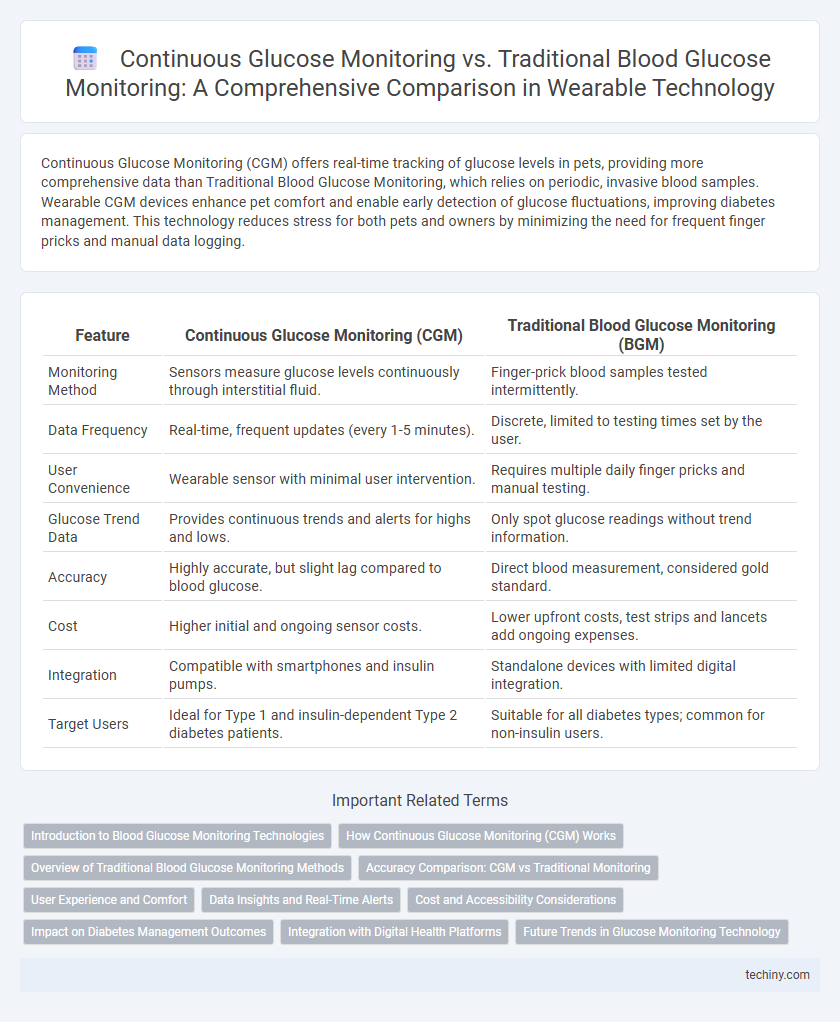
Table of Comparison
| Feature | Continuous Glucose Monitoring (CGM) | Traditional Blood Glucose Monitoring (BGM) |
|---|---|---|
| Monitoring Method | Sensors measure glucose levels continuously through interstitial fluid. | Finger-prick blood samples tested intermittently. |
| Data Frequency | Real-time, frequent updates (every 1-5 minutes). | Discrete, limited to testing times set by the user. |
| User Convenience | Wearable sensor with minimal user intervention. | Requires multiple daily finger pricks and manual testing. |
| Glucose Trend Data | Provides continuous trends and alerts for highs and lows. | Only spot glucose readings without trend information. |
| Accuracy | Highly accurate, but slight lag compared to blood glucose. | Direct blood measurement, considered gold standard. |
| Cost | Higher initial and ongoing sensor costs. | Lower upfront costs, test strips and lancets add ongoing expenses. |
| Integration | Compatible with smartphones and insulin pumps. | Standalone devices with limited digital integration. |
| Target Users | Ideal for Type 1 and insulin-dependent Type 2 diabetes patients. | Suitable for all diabetes types; common for non-insulin users. |
Introduction to Blood Glucose Monitoring Technologies
Continuous Glucose Monitoring (CGM) offers real-time tracking of glucose levels through subcutaneous sensors, providing a dynamic view of glucose fluctuations that traditional Blood Glucose Monitoring (BGM) methods, which rely on intermittent finger-prick testing, cannot deliver. CGM devices enhance diabetes management by reducing the frequency of manual testing and alerting users to hypo- or hyperglycemic episodes promptly. This technological advancement in wearable sensors significantly improves glucose control and patient adherence compared to conventional BGM systems.
How Continuous Glucose Monitoring (CGM) Works
Continuous Glucose Monitoring (CGM) utilizes a small sensor inserted under the skin to measure glucose levels in interstitial fluid every few minutes, providing real-time data throughout the day and night. This sensor wirelessly transmits glucose readings to a smartphone or dedicated receiver, enabling users to track trends and patterns without frequent finger-pricking. CGM systems enhance diabetes management by offering dynamic, continuous insights that traditional blood glucose monitoring, which relies on periodic blood samples, cannot provide.
Overview of Traditional Blood Glucose Monitoring Methods
Traditional blood glucose monitoring methods typically involve finger-prick tests using a lancet to draw a small blood sample, which is then analyzed with a glucose meter. These techniques provide discrete glucose readings at specific moments rather than continuous data, requiring frequent manual measurement to track blood sugar levels accurately. Accuracy and reliability depend on user technique and test timing, making it less convenient compared to continuous glucose monitoring systems.
Accuracy Comparison: CGM vs Traditional Monitoring
Continuous Glucose Monitoring (CGM) offers real-time glucose readings with higher accuracy due to frequent measurements every few minutes, reducing the risk of missed glucose fluctuations compared to Traditional Blood Glucose Monitoring (BGM), which relies on intermittent finger-prick tests. Studies indicate CGM devices achieve an average Mean Absolute Relative Difference (MARD) of around 9-10%, whereas traditional BGM devices typically show MARD values closer to 15-20%, indicating greater variability and less precision. Continuous data from CGM enables better glycemic trend analysis and timely interventions, improving overall diabetes management accuracy over traditional methods.
User Experience and Comfort
Continuous glucose monitoring (CGM) offers enhanced user experience and comfort by providing real-time glucose readings through a discreet sensor worn on the skin, eliminating the need for frequent finger pricks required in traditional blood glucose monitoring. The non-invasive, automated data collection in CGM reduces discomfort and inconvenience, supporting better glucose management and lifestyle flexibility. Users benefit from customizable alerts and seamless integration with smartphones, enhancing daily comfort and proactive health tracking.
Data Insights and Real-Time Alerts
Continuous glucose monitoring (CGM) devices provide real-time data insights by tracking glucose levels every few minutes, enabling immediate detection of trends and fluctuations. In contrast, traditional blood glucose monitoring relies on intermittent finger-prick tests, offering limited snapshots without continuous trend analysis. CGM systems enhance diabetes management through real-time alerts for hypo- or hyperglycemia, significantly reducing the risk of unnoticed dangerous glucose excursions.
Cost and Accessibility Considerations
Continuous glucose monitoring (CGM) systems typically involve higher upfront costs and subscription fees compared to traditional blood glucose monitors, impacting affordability for many users. However, CGM devices offer greater accessibility through real-time data transmission and remote monitoring capabilities, which can reduce the frequency of clinic visits and improve diabetes management. Traditional blood glucose monitoring remains more widely available and affordable, especially in low-resource settings where CGM technology may be limited by cost and infrastructure.
Impact on Diabetes Management Outcomes
Continuous Glucose Monitoring (CGM) significantly improves diabetes management by providing real-time glucose data, enabling timely adjustments in insulin therapy and lifestyle. Traditional Blood Glucose Monitoring (BGM) requires multiple daily finger-pricks, offering only intermittent glucose levels that may miss critical fluctuations. Studies show CGM reduces hypoglycemic events and HbA1c more effectively than BGM, leading to better long-term glycemic control and quality of life for diabetic patients.
Integration with Digital Health Platforms
Continuous glucose monitoring (CGM) devices seamlessly integrate with digital health platforms through real-time data syncing, enabling comprehensive glucose trend analysis and personalized diabetes management. Traditional blood glucose monitoring (BGM) relies on manual data entry, limiting automated insights and delaying intervention opportunities. Advanced wearables with CGM technology enhance patient engagement by providing immediate alerts and continuous feedback via smartphone apps and cloud-based health ecosystems.
Future Trends in Glucose Monitoring Technology
Continuous glucose monitoring (CGM) technology is evolving with advancements in non-invasive sensors, AI-driven analytics, and enhanced real-time data integration, promising greater accuracy and user convenience compared to traditional blood glucose monitoring. Emerging trends include the integration of CGM devices with smartwatches and mobile health platforms, enabling seamless health tracking and personalized diabetes management. Further innovations in sensor biocompatibility and extended wear times are expected to improve patient adherence and long-term glycemic control.
Continuous Glucose Monitoring vs Traditional Blood Glucose Monitoring Infographic
 techiny.com
techiny.com