Autologous biotechnology in pets uses the animal's own cells to create personalized treatments, minimizing immune rejection and enhancing safety. Allogeneic approaches involve donor cells from other animals, offering scalable options but with higher risks of immune response and rejection. Choosing between autologous and allogeneic methods depends on factors like treatment urgency, cost, and the pet's health condition.
Table of Comparison
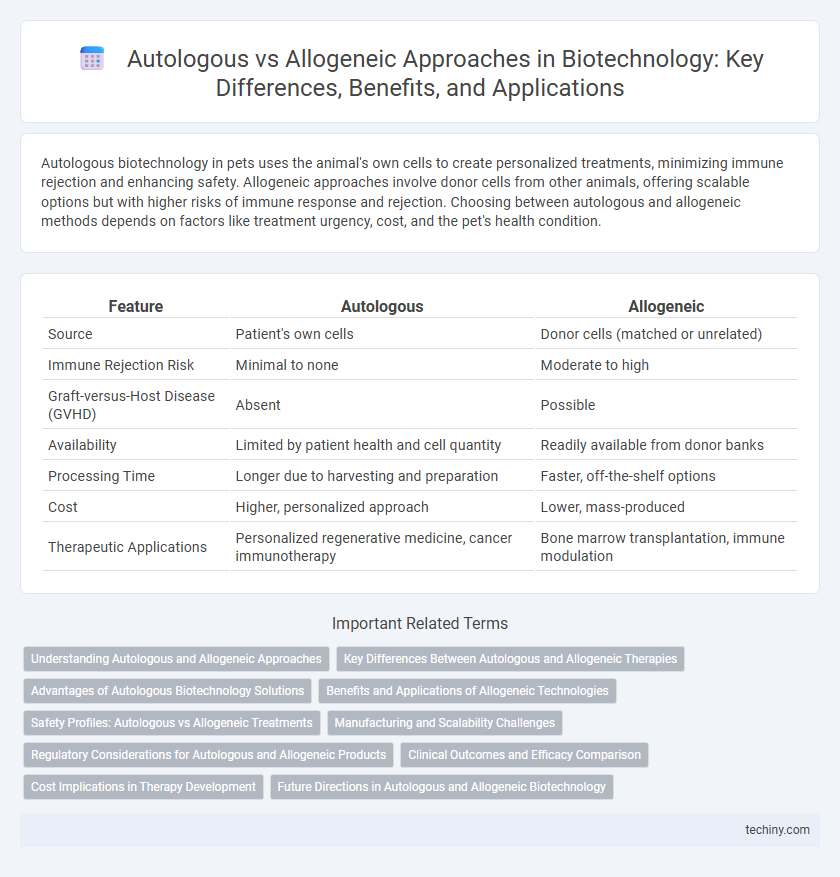
| Feature | Autologous | Allogeneic |
|---|---|---|
| Source | Patient's own cells | Donor cells (matched or unrelated) |
| Immune Rejection Risk | Minimal to none | Moderate to high |
| Graft-versus-Host Disease (GVHD) | Absent | Possible |
| Availability | Limited by patient health and cell quantity | Readily available from donor banks |
| Processing Time | Longer due to harvesting and preparation | Faster, off-the-shelf options |
| Cost | Higher, personalized approach | Lower, mass-produced |
| Therapeutic Applications | Personalized regenerative medicine, cancer immunotherapy | Bone marrow transplantation, immune modulation |
Understanding Autologous and Allogeneic Approaches
Autologous approaches in biotechnology utilize a patient's own cells, minimizing immune rejection and improving compatibility for therapies such as stem cell transplants. Allogeneic methods involve donor cells that, while more readily available and scalable, carry a higher risk of immune response complications like graft-versus-host disease. Selecting between autologous and allogeneic sources depends on factors such as treatment urgency, cell availability, and the patient's immune profile.
Key Differences Between Autologous and Allogeneic Therapies
Autologous therapies utilize a patient's own cells, minimizing immune rejection risks and eliminating the need for immunosuppressive drugs, while allogeneic therapies source cells from a donor, enabling off-the-shelf availability and broader patient access. Autologous treatments often require personalized manufacturing processes, leading to longer production times and higher costs, whereas allogeneic approaches benefit from standardized scalability and reduced manufacturing complexity. Immune compatibility remains a critical factor, with autologous cells offering perfect histocompatibility, contrasting with allogeneic cells that carry a risk of graft-versus-host disease (GVHD) and require tissue matching.
Advantages of Autologous Biotechnology Solutions
Autologous biotechnology solutions offer significant advantages such as reduced risk of immune rejection and graft-versus-host disease since the cells are derived from the patient's own body. This personalized approach enhances biocompatibility and improves treatment efficacy by using genetically matching cells. Additionally, autologous therapies often enable faster regulatory approval and lower immunosuppressive medication requirements.
Benefits and Applications of Allogeneic Technologies
Allogeneic biotechnology offers significant benefits including immediate availability, scalability, and standardized quality for therapeutic applications, making it ideal for large patient populations. These technologies enable off-the-shelf cell therapies, reducing manufacturing time and costs compared to autologous approaches. Common applications of allogeneic therapies include hematopoietic stem cell transplantation, immunotherapy for cancer, and regenerative medicine targeting chronic diseases.
Safety Profiles: Autologous vs Allogeneic Treatments
Autologous treatments, derived from the patient's own cells, minimize immune rejection risks and typically exhibit superior safety profiles compared to allogeneic therapies, which use donor cells and carry higher potential for immune-related adverse effects such as graft-versus-host disease (GVHD). Rigorous screening and immunosuppressive protocols are essential in allogeneic treatments to mitigate risks and improve patient outcomes. Advances in CRISPR gene-editing and cell-matching technologies continue to enhance the safety and efficacy of both autologous and allogeneic approaches in regenerative medicine and cell therapy.
Manufacturing and Scalability Challenges
Autologous cell therapies face manufacturing challenges due to individualized processing, leading to higher costs and extended production times. Allogeneic therapies offer improved scalability by enabling mass production from a single donor source, but they require rigorous immune compatibility testing and stringent quality control. Balancing batch consistency and regulatory compliance remains critical for both approaches to ensure therapeutic efficacy and patient safety.
Regulatory Considerations for Autologous and Allogeneic Products
Regulatory considerations for autologous products emphasize stringent controls on cell sourcing and minimal manipulation to ensure patient-specific safety and efficacy. Allogeneic products face rigorous evaluation for immunogenicity, donor compatibility, and scalable manufacturing processes under regulatory frameworks such as the FDA's 21 CFR Part 1271. Both product types require compliance with Good Manufacturing Practices (GMP) and thorough clinical trial data to address risks related to contamination, immune reactions, and long-term safety.
Clinical Outcomes and Efficacy Comparison
Autologous cell therapies demonstrate higher biocompatibility and reduced immune rejection, resulting in improved clinical outcomes such as enhanced tissue regeneration and lower incidence of graft-versus-host disease. Allogeneic therapies offer scalable off-the-shelf solutions but may exhibit variable efficacy due to immune incompatibility, often necessitating immunosuppressive regimens that can impact patient safety. Comparative studies reveal autologous treatments generally provide superior long-term efficacy, although allogeneic cells facilitate broader applicability and rapid availability in clinical settings.
Cost Implications in Therapy Development
Autologous cell therapies involve harvesting and engineering a patient's own cells, resulting in higher production costs due to personalized manufacturing and complex logistics. Allogeneic therapies use donor cells, enabling scaled-up production and reduced per-unit expenses, though initial R&D and immune compatibility testing can be substantial. Cost implications directly impact market pricing, investment in clinical trials, and accessibility of advanced regenerative treatments.
Future Directions in Autologous and Allogeneic Biotechnology
Future directions in autologous biotechnology emphasize personalized cell therapies using patient-derived cells to enhance compatibility and reduce immune rejection. Allogeneic biotechnology advances focus on developing universal donor cell lines with gene editing technologies to minimize graft-versus-host disease and enable off-the-shelf therapeutic applications. Combining both approaches, researchers aim to optimize efficacy, scalability, and accessibility of regenerative medicine products.
autologous vs allogeneic Infographic
 techiny.com
techiny.com